
Gonarthrosisis deforming arthrosis of the knee joint. It is accompanied by damage to the hyaline cartilage of the articular surfaces of the tibia and femur and has a chronic progressive course. Clinical symptoms include pain that worsens with movement, limitation of movement, and synovitis (fluid buildup) in the joint. In the later stages, leg support is compromised and marked limitation of movement is observed. The pathology is diagnosed on the basis of medical history, complaints, physical examination and x-ray of the joint. Treatment is conservative: drug therapy, physiotherapy, physical therapy. If there is significant destruction of the joint, endoprosthesis is indicated.
general informations
Gonarthrosis (from the Latin articulatio genus - knee joint) or deforming arthrosis of the knee joint is a progressive degenerative-dystrophic lesion of the intra-articular cartilage of a non-inflammatory nature. Gonarthrosis is the most common osteoarthritis. It usually affects middle-aged and elderly people, women are more often affected. After an injury or intense and constant stress (for example during professional sports), gonarthrosis can occur at a young age. Prevention plays the most important role in preventing the onset and development of gonarthrosis.
Contrary to popular belief, the cause of the development of the disease lies not in the deposition of salts, but in malnutrition and changes in the structure of intraarticular cartilage. In gonarthrosis, foci of calcium salt deposits may occur at the insertion site of the tendon and ligament system, but they are secondary and do not cause painful symptoms.
Causes of gonarthrosis
In most cases, it is impossible to identify a reason for the development of pathology. As a rule, the onset of gonarthrosis is caused by a combination of several factors, including:
- Injuries. Approximately 20-30% of cases of gonartosis are associated with previous injuries: fractures of the tibia (especially intra-articular), meniscal injuries, tears or ruptures of the ligaments. Usually, gonarthrosis occurs 3-5 years after a traumatic injury, although earlier development of the disease is possible - 2-3 months after the injury.
- Physical exercise. Often the manifestation of gonarthrosis is associated with excessive loads on the joint. The age after 40 is a time when many people understand that regular physical activity is necessary to keep the body in good condition. When starting to exercise, they do not take into account age-related changes and unnecessarily load the joints, which leads to the rapid development of degenerative changes and the appearance of symptoms of gonarthrosis. Fast, intense running and squats are especially dangerous for knee joints.
- Excess weight. With excess body weight, the load on the joints increases, both microtraumas and serious damage (meniscus rupture or ligament rupture) occur more often. Gonarthrosis is especially difficult in obese patients with severe varicose veins.
The risk of gonarthrosis also increases after previous arthritis (psoriatic arthritis, reactive arthritis, rheumatoid arthritis, gouty arthritis or ankylosing spondylitis). In addition, risk factors for the development of gonarthrosis include genetically determined weakness of the ligament system, metabolic disorders and impaired innervation in some neurological diseases, traumatic brain injuries and spinal injuries.
Pathogenesis
The knee joint is formed by the articular surfaces of two bones: the femur and the tibia. On the anterior surface of the joint is the patella, which, when moving, slides along the depression between the condyles of the femur. The fibula does not participate in the formation of the knee joint. Its upper part is located on the side, just below the knee joint and is connected to the tibia via a low-motion joint.
The articular surfaces of the tibia and femur, as well as the posterior surface of the patella, are covered with smooth, very strong and elastic densely elastic hyaline cartilage 5-6 mm thick. Cartilage reduces friction forces during movements and performs a shock-absorbing function during shock loads.
In the first stage of gonarthrosis, blood circulation in the small intraosseous vessels supplying the hyaline cartilage is interrupted. The surface of the cartilage becomes dry and gradually loses its smoothness. Cracks appear on its surface. Instead of sliding smoothly and unhindered, the cartilages "cling" to each other. Due to continuous microtraumas, the cartilaginous tissue becomes thinner and loses its shock-absorbing properties.
In the second stage of gonarthrosis, compensatory changes occur in bone structures. The articular platform is flattened, adapting to greater loads. The subchondral area (the part of the bone located immediately under the cartilage) thickens. Along the edges of the joint surfaces, bone growths appear - osteophytes, which in their appearance on the x-ray resemble spines.
During gonarthrosis, the synovial membrane and joint capsule also degenerate and become "wrinkled". The nature of the joint fluid changes: it thickens, its viscosity increases, which leads to a deterioration of its lubricating and nutritional properties. Due to lack of nutrients, cartilage degeneration accelerates. The cartilage becomes even thinner and in some areas disappears completely. After the disappearance of the cartilage, the friction between the joint surfaces increases significantly, and the degenerative changes progress rapidly.
In the third stage of gonarthrosis, the bones are significantly deformed and appear to be pressed into each other, significantly limiting the movement of the joint. The cartilaginous tissue is practically absent.
Classification
Taking into account the pathogenesis in traumatology and orthopedics, two types of gonarthrosis are distinguished: primary (idiopathic) and secondary gonarthrosis. Primary gonarthrosis occurs without prior trauma in elderly patients and is usually bilateral. Secondary gonarthrosis develops against the background of pathological changes (diseases, developmental disorders) or injuries of the knee joint. It can occur at any age, usually unilateral.
Taking into account the severity of pathological changes, three stages of gonarthrosis are distinguished:
- First stage– initial manifestations of gonarthrosis. Characterized by periodic dull pain, usually after significant load on the joint. You may experience slight swelling of the joint that goes away on its own. There is no deformation.
- Second phase– increase in symptoms of gonarthrosis. The pain becomes longer and more intense. A creaking sound often appears. There is mild to moderate limitation of movement and slight deformation of the joint.
- Third phase– the clinical manifestations of gonarthrosis reach their maximum. The pain is almost constant, the gait is impaired. There is a pronounced limitation of mobility and noticeable deformation of the joint.
Symptoms of gonarthrosis
The disease begins gradually, gradually. In the first stage of gonarthrosis, patients feel mild pain during movements, especially when going up or down stairs. You may experience a sensation of joint stiffness and "tightening" in the popliteal area. A characteristic symptom of gonarthrosis is "initial pain" - painful sensations that occur during the first steps after getting up from a sitting position. When a patient with gonarthrosis "diverges", the pain decreases or disappears and reappears after significant stress.
Externally the knee has not changed. Sometimes patients with gonarthrosis notice a slight swelling of the affected area. In some cases, in the first stage of gonarthrosis, fluid accumulates in the joint - synovitis develops, characterized by an increase in the volume of the joint (it becomes swollen, spherical), a feeling of heaviness and limitation of movements.
In the second phase of gonarthrosis, the pain becomes more intense, manifests itself even with light loads and intensifies with intense or long walks. As a rule, the pain is localized along the anterior inner surface of the joint. After a long rest, painful sensations usually disappear and reappear with movement.
As gonarthrosis progresses, the range of motion of the joint gradually decreases, and when trying to bend the leg as much as possible, sharp pain appears. There may be a grinding noise when moving. The configuration of the joint changes, as if it is expanding. Synovitis appears more often than in the first stage of gonarthrosis and is characterized by a more persistent course and the accumulation of more fluids.
At the third stage of gonarthrosis, the pain becomes almost constant, disturbing patients not only when walking, but also at rest. In the evening, patients spend a lot of time trying to find a comfortable sleeping position. Often the pain also appears at night.
Flexion of the joint is significantly limited. In some cases, not only flexion, but also extension is limited, which is why the patient with gonarthrosis cannot fully straighten the leg. The joint is enlarged and deformed. Some patients have hallux valgus or varus deformities: the legs take on the shape of an X or an O. Due to limited movement and deformation of the legs, the gait becomes unstable and sways. In more severe cases, patients suffering from gonarthrosis can only move with the support of a cane or crutches.
Diagnostics
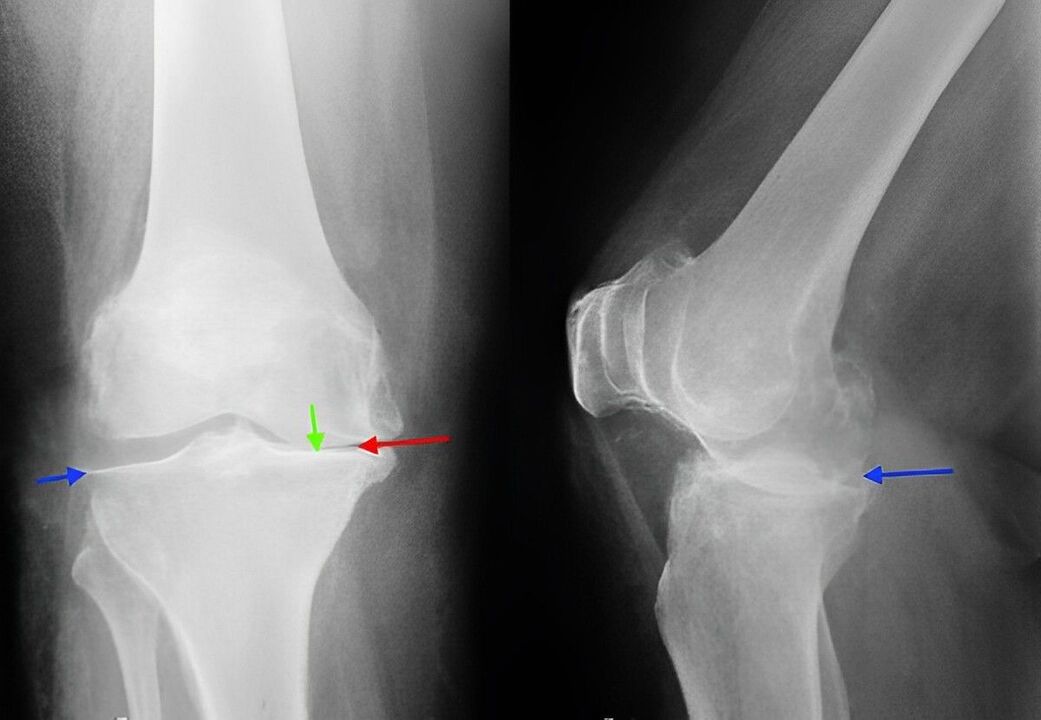
The diagnosis of gonarthrosis is made on the basis of the patient's complaints, physical examination data and radiographic examination. When examining a patient with gonarthrosis in the first stage, it is usually not possible to detect external changes. In the second and third stages of gonarthrosis, enlargement of the contours of the bones, deformation of the joint, limitation of movements and curvature of the axis of the limb are detected. When the kneecap moves in the transverse direction, a creaking sound is heard. Palpation reveals a tender area towards the inside of the kneecap, at the level of the joint space, as well as above and below it.
With synovitis, the joint increases in volume, its contours become smooth. A swelling is noted along the anterolateral surfaces of the joint and over the patella. Fluctuation is determined by palpation.
Knee joint radiography is a classic technique that allows you to clarify the diagnosis, establish the severity of pathological changes in gonarthrosis and monitor the dynamics of the process, taking repeated images after some time. Thanks to its availability and low cost, it still remains the main method for diagnosing gonarthrosis today. In addition, this research method allows you to exclude other pathological processes (for example, tumors) in the tibia and femur.
In the initial stage of gonarthrosis, changes on radiographs may be absent. Subsequently, there is a narrowing of the joint space and a compaction of the subchondral area. The articular ends of the femur and especially the tibia expand, the edges of the condyles become pointed.
When studying an x-ray, it should be taken into account that in most elderly people, more or less pronounced changes characteristic of gonarthrosis are observed and are not always accompanied by pathological symptoms. The diagnosis of gonarthrosis is made only with a combination of radiological and clinical signs of the disease.
Currently, along with traditional radiography, modern techniques such as computed tomography of the knee joint, which allows a detailed study of pathological changes in bone structures, and magnetic resonance imaging of the knee joint, used to identify changes in the soft tissues. .
Treatment of gonarthrosis
Conservative activities
Treatment is carried out by traumatologists and orthopedists. Therapy for gonarthrosis should begin as soon as possible. During the period of exacerbation, the patient with gonarthrosis is advised to rest for maximum unloading of the joint. The patient is prescribed therapeutic exercises, massages, physiotherapy (UHF, electrophoresis with novocaine, phonophoresis with hydrocortisone, diadynamic currents, magnetic and laser therapy) and mud therapy.
Drug therapy for gonarthrosis includes chondroprotectors (drugs that improve metabolic processes in the joint) and drugs that replace synovial fluid. In some cases, with gonatrosis, intra-articular administration of steroid hormones is indicated. Subsequently, the patient can be referred to sanatorium treatment.
A patient suffering from gonarthrosis may be advised to walk with a cane to unload the joint. Sometimes special orthoses or custom orthotics are used. To slow down the degenerative processes of the joint with gonarthrosis it is very important to follow some rules: physical exercise, avoiding unnecessary stress on the joint, choosing comfortable shoes, monitoring your weight, adequately organizing your daily routine (alternating load and rest, performing special exercises) .
Surgery
With pronounced destructive changes (at the third stage of gonarthrosis), conservative treatment is ineffective. In case of severe pain, joint dysfunction and limited working capacity, especially if a young or middle-aged patient suffers from gonarthrosis, surgery (knee replacement) is resorted to. Rehabilitation measures are subsequently carried out. The period of complete recovery after joint replacement surgery for gonarthrosis lasts from 3 months to six months.




































